- Cutting-edge brain implant enables people with paralysis to move and feel again
- New device allows the visually impaired to ‘see’
- Brain-computer interface can predict epileptic seizures
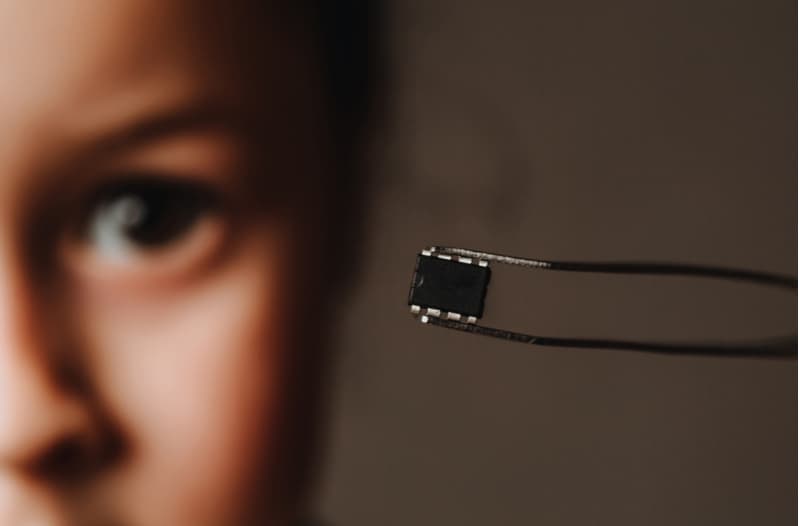
- The ultimate medical treatment could be a computer chip
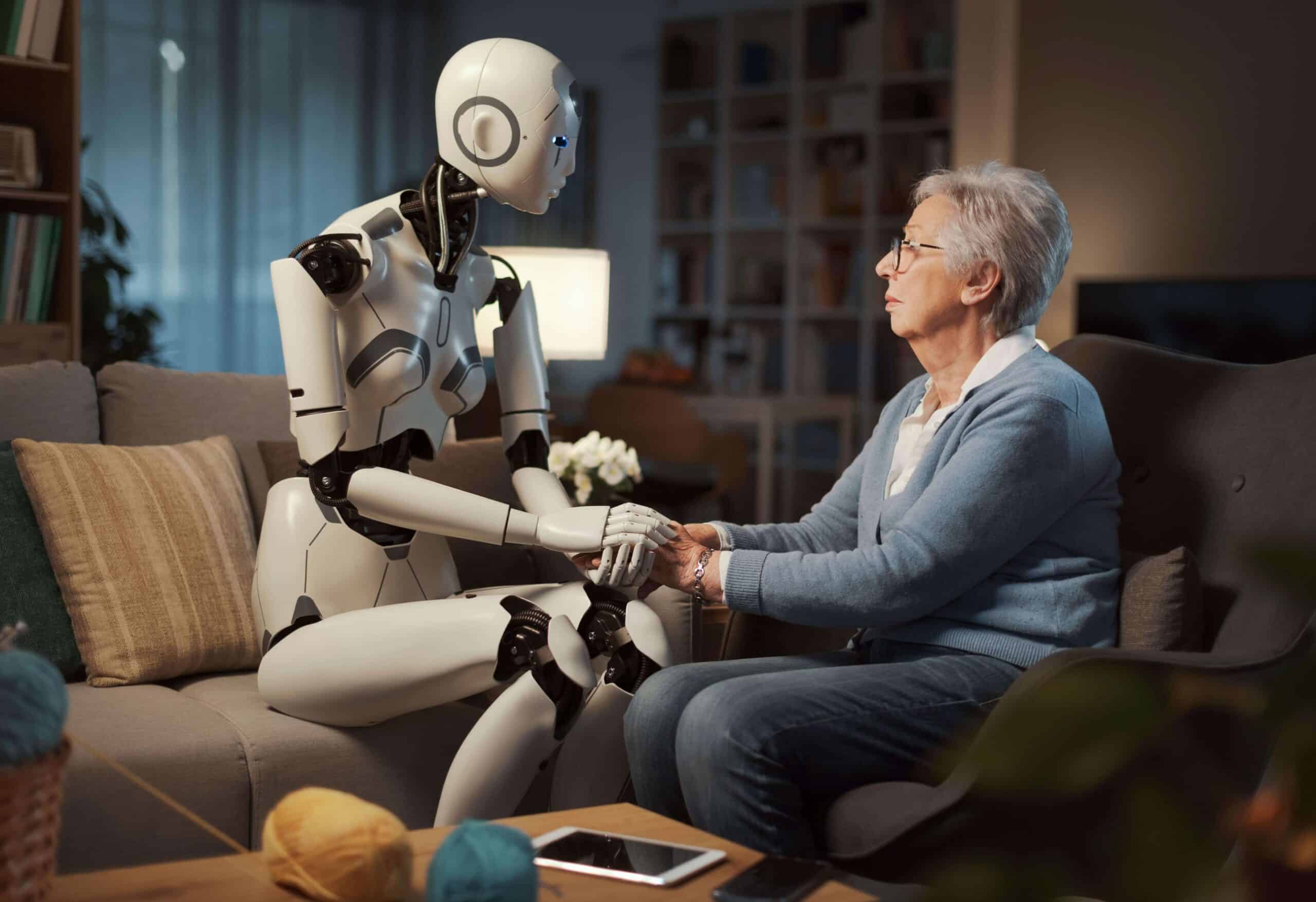
A discouragingly large number of people are affected by some form of paralysis. In fact, this is more widespread than previously thought. According to the 2019 National SCI Statistical Centre Data Sheet, every year, nearly 18 thousand new spinal cord injuries are reported in the US. Similarly, Western European countries report 16 to 19.4 new traumatic spinal cord injuries per million inhabitants every year. And globally, more than a billion people are affected by some form of physical disability. Thanks to advances in technology, however, people living with paralysis could soon see changes in their circumstances.
The 2020 research report Global Disabled and Elderly Assistive Technology Industry estimates that the global disabled and elderly assistive technology market is about to reach a value of $31.5 billion by 2027. Assistive devices and technologies have become more cutting-edge and sophisticated in design. This means that ever-evolving solutions already on the market – and those still being tested in labs – could soon help disabled people to reduce their dependence on others and improve their quality of life.
Cutting-edge brain implant enables people with paralysis to move and feel again
Paralysis is accompanied by the lack of sensation in the body, which makes it impossible for the affected to move and feel. Movement restriction and often full dependency on assistive devices or caretakers significantly lowers quality of life. Not being able to enjoy activities they enjoyed before – for instance, as a result of an accident – can be devastating. This was the case with freshman Ian Burkhart, who suffered a spinal cord injury (SCI) in 2010. The injury caused him to completely lose his sense of touch, although he retained a limited amount of motion in his shoulder and biceps. After years of adjusting to this new life, Burkhart was willing to undergo an experimental procedure and participate in a program called NeuroLife at Battelle, an Ohio-based, nonprofit research organisation, to improve the range of motion in his arms and to artificially recreate his sense of touch. “Helping people to become more whole again and less dependent on caregivers is a major step in improving quality of life,” said Justin Sanchez, a Battelle Life Sciences Technical Fellow. Burkhart was happy to give it a try, even if there was only a slight chance that he could regain the ability to walk or feel again. “It was a lot to consider, but paralysis wasn’t something I was ready to settle for.”
In 2014, at Ohio State University’s Wexner Medical Center, a chip the size of a grain of rice was surgically implanted close to Burkhart’s primary motor cortex – the main contributor to generating neural impulses that pass down to the spinal cord and control the execution of movement. This way, the minute yet powerful device was able to monitor electrical signals from the primary motor cortex. Six years after the implantation of the chip, Burkhart can feel objects and has enough control over his arm to play video games like Guitar Hero. “When the chip was placed on the surface of Ian’s motor cortex in 2014, it was not known that the signals related to object touch could be observed because of the paralysis. Furthermore, Burkhart has a very severe SCI that should essentially block hand touch signals from even reaching the brain.”
A few wisps of Burkhart’s spinal fibres survived, and using “even that small contingent of fibers lead to a reasonable signal in the brain,” says Patrick Ganzer, a neuroscientist at Battelle. The team extracted those weak signals from the brain, decoded their meaning, and relayed them to the limbs, bypassing the spine and reconnecting the brain and body. The trial has demonstrated that, regardless of the severity of the spinal cord injury, there’s still a high probability that people with paralysis could soon be able to regain full mobility and their sense of touch.
New device allows the visually impaired to ‘see’
We’ve already mentioned breakthroughs in science that could soon help the paralysed regain their mobility and sense of touch, but when it comes to enabling visually impaired people to see, BCI tech is still not ‘quite there yet’. And worldwide, there are more than 2 billion people with some degree of visual impairment or blindness. This number, however, could soon decrease thanks to some recent innovative solutions. A research team from the University of Miguel Hernandez de Elche in Spain, for instance, has developed a 100-electrode implant for placement in the visual cortex.
The first patient to undergo surgery was Bernadeta Gómez, a 57-year old lady who has been blind for the past 15 years. At the age of 42, she was diagnosed with toxic optic neuropathy, a condition that cuts off the connection between the brain and the eyes, leading to blindness. But now, thanks to the implant, she has regained some sight. The system comprises a set of glasses with a small camera that captures the wearer’s surroundings. The camera sends live video to a computer that turns the images into electrical signals. The signals are then sent to the visual cortex where they create a rough image.
Gomez now ‘sees’ the world through phosphenes, the phenomenon of seeing light without light actually entering the eye. Images re-created in the visual cortex this way are, however, of poor resolution – around 10×10 pixels – which isn’t a high enough resolution to see details like facial features. Incorporating facial recognition software and sending the corresponding phosphenes to Gomez’s brain, however, enabled her to learn to associate these with the images of specific persons.
Another flaw of the implant is that it tends to decay in the living tissue, which means that it can only stay in the cortex for a limited period of time. Even so, the device might offer millions of blind people at least a bit of hope. Neuroengineer Eduardo Fernandez, who led the research, says, “We [soon] hope to have a system people can use, but right now we’re just conducting early experiments.”
Brain-computer interface can predict epileptic seizures
Any degree of disability can affect your quality of life. Epilepsy, for instance, one of the most common neurological diseases, can affect people of all ages. Some forms are caused by a disease or an accident, while others are congenital. As many as 50 million people around the world suffer from epilepsy. If diagnosed early and treated the right way, epilepsy can be managed well. In some cases, people can even become seizure-free. Unfortunately, it’s estimated that “three quarters of people with epilepsy living in low-income countries do not get the treatment they need”. Also, the risk of premature death in people with epilepsy is three times higher than in healthy people.
In 2018, the California-based medical technology company NeuroPace Inc. announced the launch of its flagship technology – the next-gen responsive neurostimulation (RNS) system. After years of developing the technology, the device that uses BCI is designed in such a way that it continuously monitors the patients’ brain waves in order to recognise unique seizure onset fingerprints. This means that each patient will get to know their own seizure onset patterns, enabling them to prevent them from happening, which is done by the device’s response with imperceptible electric pulses. NeuroPace CEO Frank Fischer is optimistic and shares his excitement over the company’s achievements. “The launch of the next-gen RNS System is proof of our relentless focus on product innovation. According to the National Epilepsy Foundation, 1 in 26 Americans will develop epilepsy in their lifetime, with approximately 150,000 new cases of epilepsy diagnosed annually. An estimated 3 million Americans currently live with epilepsy, with one-third of those patients experiencing seizures despite taking epilepsy medication. The RNS System is a proven treatment option for individuals 18 years of age or older who have disabling partial onset seizures that are not controlled by medication.”
More good news from the company is that their RBS System, “a closed-loop brain-responsive neurostimulation system designed to prevent seizures in adults refractory to anti-seizure medications”, has finally received FDA approval for MRI labelling. For patients this means that they managed to “remove a potential barrier to treatment, increasing the number of patients who can benefit from this life-changing therapy.”
The ultimate medical treatment could be a computer chip
Though rather small – no larger than a grain of rice – chips can be extremely powerful. They could help people with disabilities regain mobility and their sense of touch and help people struggling with visual impairment regain (some) sight. BCI-based systems have also been proven effective in the treatment of conditions like epilepsy, which is especially important for those who don’t optimally respond to existing medical treatment. BCI-based solutions could be used for numerous brain disorders, including Alzheimer’s, and help in early prediction, diagnosis, and the development of highly effective treatments. Welcome to the future, where the ultimate medical treatment could be a computer chip.